New Paragraph
Frequently asked Questions
Tips & Advise from our Pediatricians
What is the recommended vaccination schedule for my child?
At Pediatric Services of Springfield
the health of your child is our priority.
We follow the U.S. Center for Disease Control and
Prevention recommended vaccination guidelines.
As your healthcare provider we strive to provide you
detailed education and understanding of the importance
of all recommended vaccinations. The CDC provides
VIS vaccination information statements on each vaccine.
At your child's wellness appointment we will provide
the VIS on each vaccination administered
and answer any questions and
concerns you may have.
Does my child have a fever? How do I check my child's temperature?
How do I care for my child with diarrhea and/or vomiting?
Dosing Charts for Infants and Children
Below are pediatric dosing charts for Tylenol (Acetaminophen) and Motrin (Ibuprofen). This information is not intended to be a substitute for professional medical advice. Please contact our office with questions or concerns 413-525-1870.
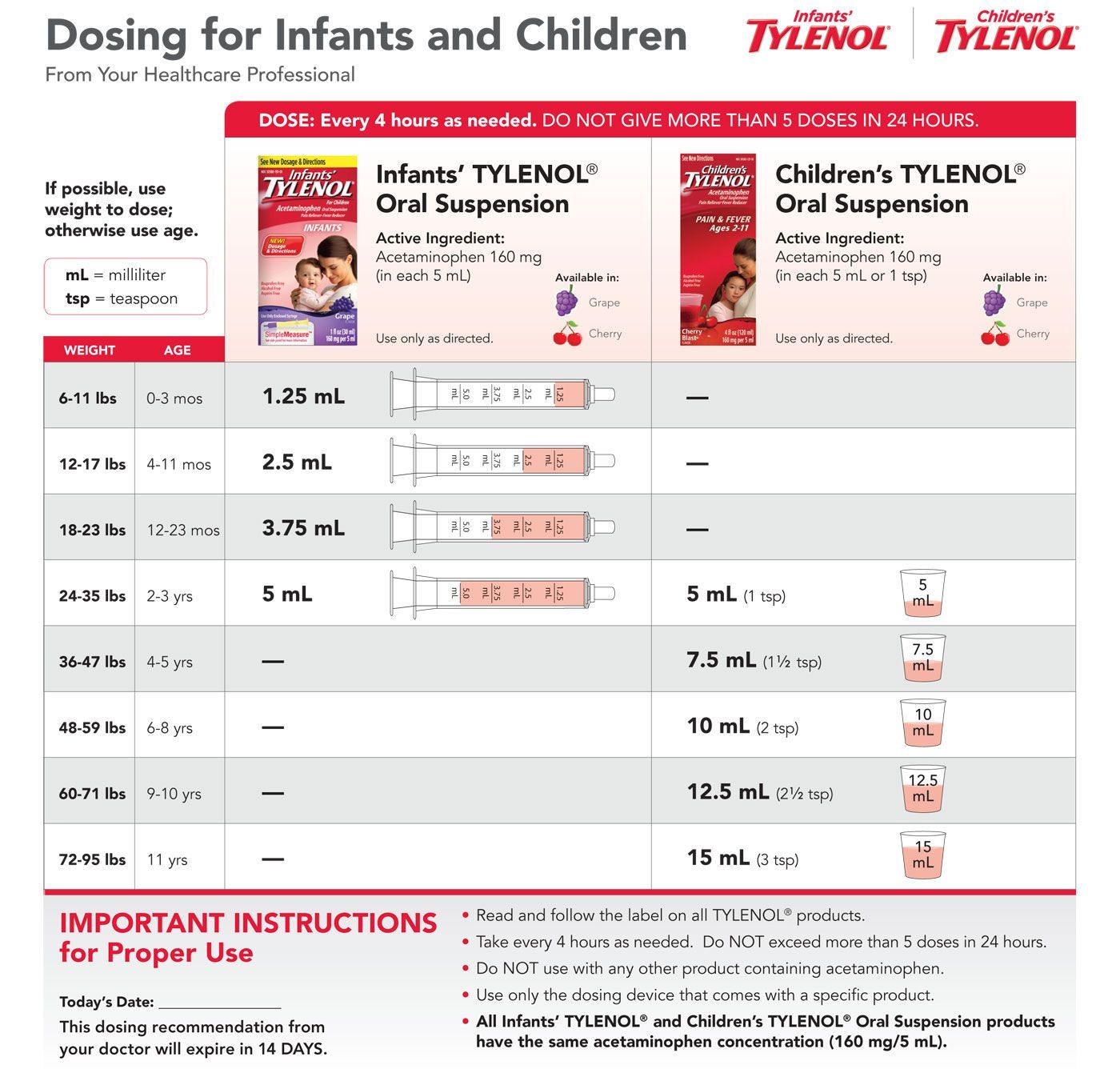
Tylenol (Acetaminophen):
Repeat every 4-6 hours as needed or as directed by your doctor. Do not exceed more than 5 doses in a 24 hour period.
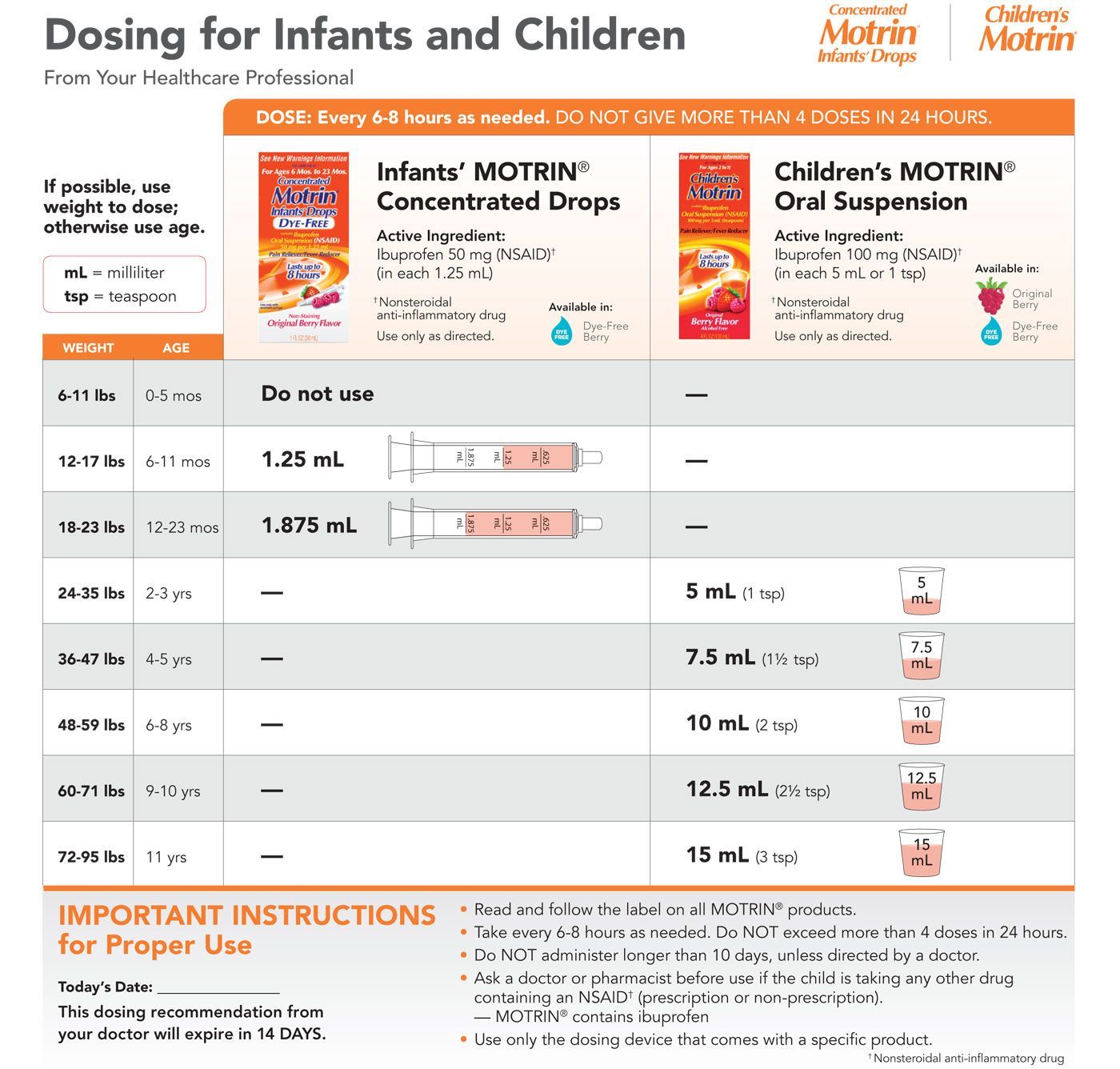
Motrin (Ibuprofen):
Do not use Ibuprofen under 6 months of age unless directed by your doctor.
Infants and children 6 months of age and over repeat every 6-8 hours as needed or as directed by your doctor. Do not exceed more than 4 doses in 24 hour period.
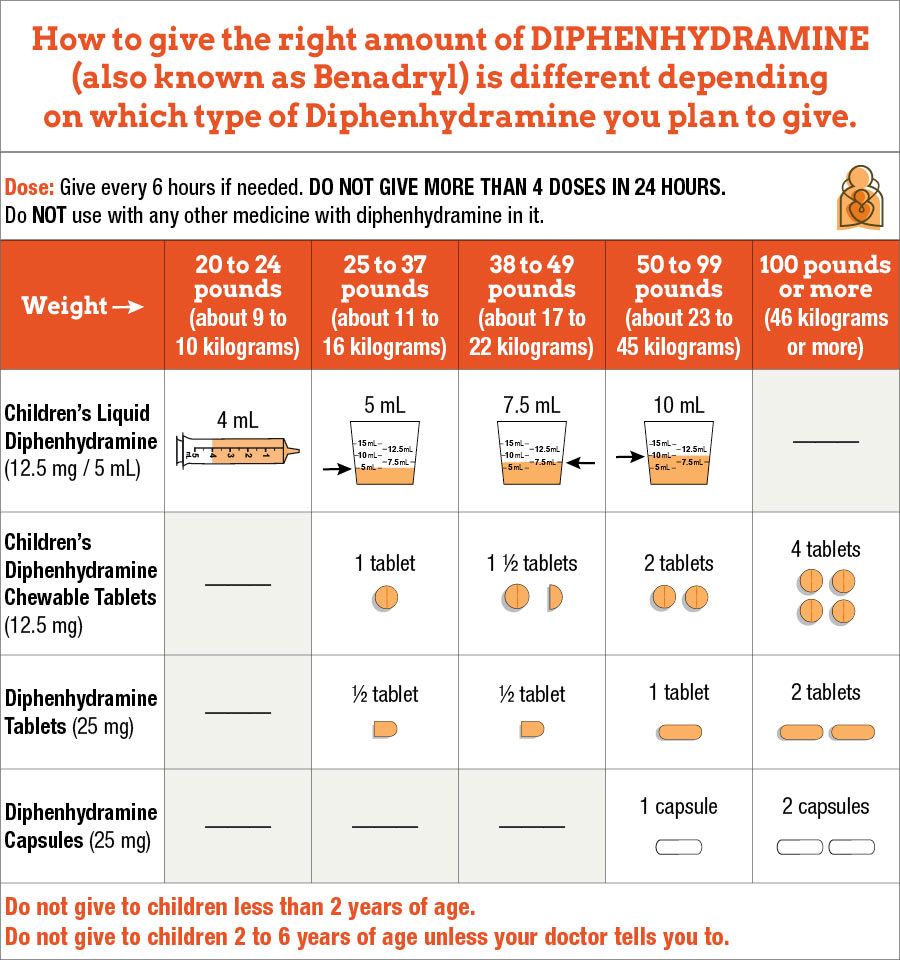
Benadryl (diphenhydramine):
Do not use
Benadryl (diphenhydramine) under 2 years of age.
Do not use
Benadryl (diphenhydramine) ages 2-6 years of age
unless directed by your doctor.
Children 2 years of age and over repeat every 6 hours if needed/as directed by your doctor. Do not exceed more than 4 doses in 24 hour period.